Peri-implantitis is a complex subject, so we thought it would be useful to give an anatomical and historical overview of periodontal and peri-implant tissues as well as periodontal and peri-implant pathologies in order to better understand the physiopathology of peri-implantitis.
In the second article of this series, we will focus on peri-implantitis itself, its epidemiological data, the different means of diagnosis and the different risk factors.
Finally, the last article will deal with curative and preventive therapies.
Periodontal tissues and peri-implantitis
The gum
The gum is one of the soft tissues lining the oral cavity. It is a keratinised epithelial-conjunctive entity (except in the region of the interdental neck) which extends from the marginal part to the muco-gingival line. Its thickness is of the order of one millimetre and depends essentially on the height of the gum, the type and position of the teeth.
The deep periodontium
The deep periodontium consists of :
- The Cementum.
- The Alveolar ligament (Desmodont).
- The Alveolar bone.
It is separated from the gum by the biological width.
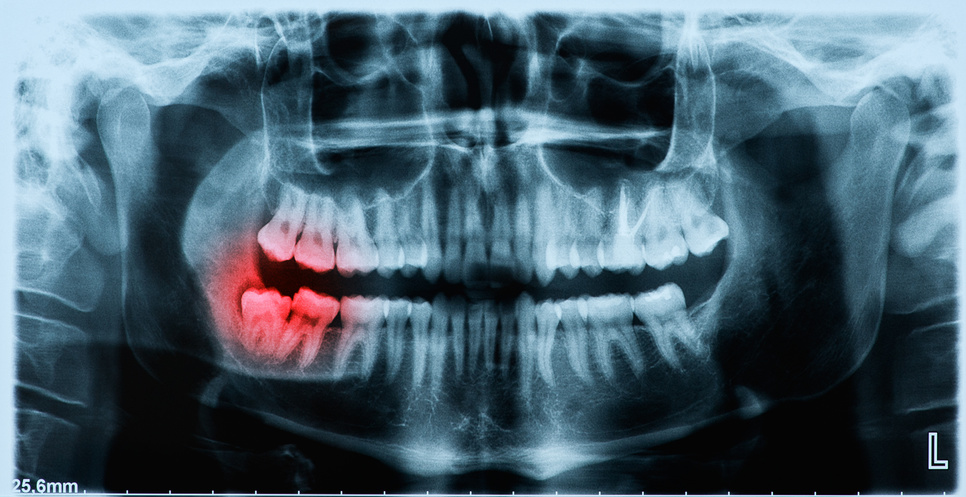
Biological width
Maynard, Wilson, Gargiulo, et al (1961) defined the biological width as the space necessary to accommodate the superficial periodontal attachment system and they carefully detail its composition and average dimensions.
The biological width is comprised between the bottom of the dental sulcus and the top of the bony ridge. This space circles the entire tooth over a height of 2mm.
It is composed of two distinct structures which follow each other and which are:
- The epithelial attachment or junctional epithelium,0.97mm high.
- The conjunctival attachment or gingival-cementary fibres, 1.07mm high.
Deep periodontium and biological width.
Schroeder, et al described the orientations of the gingival fibres and confirmed the presence of the following conformations :
Dento-gingival, dento-periosteal, alveolo-gingival and periosteal fibre groups that attach the gingiva to the teeth and bone; inter-papillary fibres that connect the vestibular and oral interdental papillae, and circular or semicircular transgingival and transeptal fibre bundles that connect the teeth to each other.
The presence of these different fibres makes the epithelial and connective attachment relatively resistant to external aggression and thus protects the deep periodontium.
Peri-implant tissues
Peri-implant tissues are the tissues surrounding the dental implants:
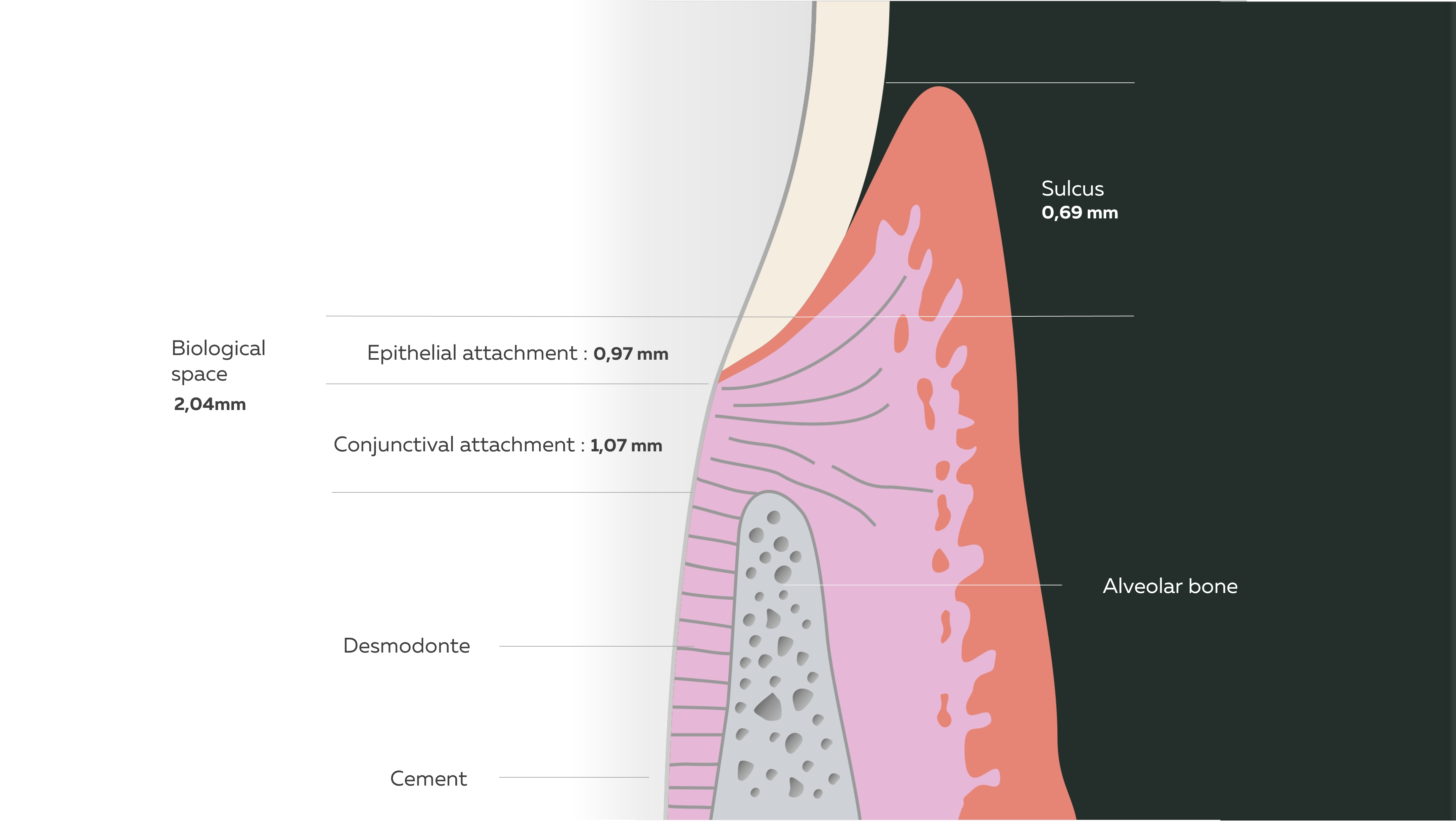
Peri-implant hard tissue and osteointegration
Alveolar bone surrounding the dental implant
The implant is held in the bone by the phenomenon of osseointegration. This phenomenon was described in 1969 by Dr. Branemark. It is considered as a functional ankylosis due to the formation of new bone on the implant surface following a process of membranous ossification. This intimate contact between the bone and the implant surface is the expected result of any implant surgery. However, this ossification greatly reduces the mobility of the implant due to the absence of a ligament, unlike a natural tooth.
Soft tissues
Also known as peri-implant mucosa
The peri-implant mucosa forms a barrier between the oral environment and the peri-implant bone tissue. It consists of an epithelial attachment containing circular fibres holding the tissue around the transmucosal region of the implants. The underlying connective tissue is poorly vascularised and rich in fibroblasts that interpose between the collagen fibres.
The connective tissue fibres are mainly organised in a circular form and oriented in a direction parallel to the implant surface. Unlike dental structures, there are no fibres perpendicular to the implant surface.

Difference between natural and implant junctional tissue.
Difference between periodontal and peri-implant tissues.
Periodontal and peri-implant disease
Periodontal and peri-implant health is characterised by the absence of inflammation, spontaneous or probing bleeding and the absence of suppuration.
Mucositis and gingivitis
Peri-implant mucositis was defined during the first European Periodontology Workshop as a reversible inflammatory reaction of peri-implant tissues. It is characterised by redness, swelling and bleeding of the peri-implant mucosa. Gingivitis, on the other hand, affects the gums and has the same clinical manifestations.
Periodontitis
This is a pathology of infectious origin that affects the supporting tissues of the tooth. It is characterised by a progressive gingival inflammation with a destruction of the bone and the alveolar ligaments, leading to dental mobility, which can in turn lead to tooth loss.
Peri-implantitis
Peri-implantitis is a pathological condition of the peri-implant tissues associated with dental plaque, characterised by inflammation of the peri-implant mucosa and progressive loss of the supporting bone. Peri-implantitis sites show signs of inflammation: probing, suppuration, pocket formation, mucosal recession and radiographic bone loss.

Saïd BOUTOUGHMAS
Dentist and quality and regulatory affairs officer at HYGITECH.
Sources
Borghetti A, Monnet-Corti V : Chirurgie plastique parodontale. 2e édition. 2-RATEISCHAK H & E.M., WOLF H.F., HASSELL T.M. Atlas de parodontologie Paris : Flammarion, 1985.
De Rosentiel, Land, Fujimoto : Contemporary fixed prosthodontics, fifth edition, 2016
Ivanovski S, Lee R : Comparison of peri-implant and periodontal marginal soft tissues in health and disease. Periodontol 2000. févr 2018;76(1):116‑30.
Chai WL, Razali M, Moharamzadeh K, Zafar MS : The hard and soft tissue interfaces with dental implants. In: Dental Implants [Internet]. Elsevier; 2020 [cité 20 avr 2021]. p. 173‑201.
Zitzmann NU, Berglundh T : Definition and prevalence of peri-implant diseases. J Clin Periodontol. sept 2008; 35:286‑91.
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, et al : Peri-implant diseases and conditions. J Periodontol. juin 2018;89: S313‑8.