Tapis de décontamination (4 x 30 feuilles)
- Karton mit 4 Matten à 30 Einwegfolien Karton mit 4 Matten à 30…
Nous contacter : 01 48 01 32 89

HYGITECH Academy invites you to watch this clinical case on dental implant placement after bone...



Pre-disinfection is the essential first step in the sterilization chain of medical and surgical instruments, particularly in dental implantology. It takes place immediately after the use of a medical device (MD) and aims to limit contamination of personnel, surfaces, and other instruments.
According to the recommendations of the Haute Autorité de Santé (HAS) and ANSM guidelines, pre-disinfection is defined as the initial treatment of medical devices after use, combining preliminary cleaning with the beginning of antimicrobial action. Its main objectives are:
to reduce microbial load prior to cleaning and sterilization,
to prevent the formation of biofilm,
to protect healthcare workers handling contaminated instruments,
to preserve the integrity of the materials by minimizing corrosion or degradation.
Timing is critical: it must be carried out immediately after the procedure, directly in the treatment room or as close as possible to the surgical field. If delayed, organic matter (blood, tissue, saliva) can dry and adhere to instruments, making later cleaning more difficult and less effective.
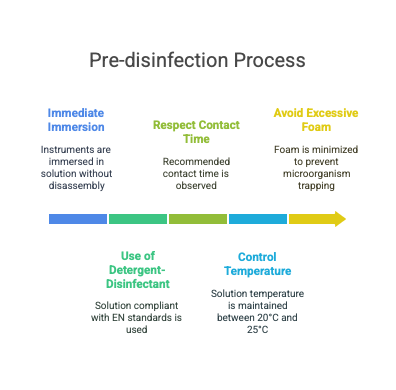
Immediate immersion of instruments in a pre-disinfection solution, without disassembly at this stage to avoid injury.
Use of a detergent-disinfectant solution compliant with EN 13727 (bactericidal activity) and EN 13624(fungicidal activity), and EN 14476 if virucidal activity is required.
Respecting the contact time recommended by the manufacturer, typically 10 to 15 minutes.
Controlled temperature of the solution (ideally between 20°C and 25°C) to ensure effectiveness without damaging materials.
Avoiding excessive foam, which may trap microorganisms and reduce product efficiency.
Change the solution between each cycle to avoid dilution or cross-contamination.
Wear appropriate personal protective equipment (PPE): resistant gloves, protective eyewear, long-sleeved gown.
Use suitable trays (stainless steel or medical-grade plastic) with a lid to prevent aerosolization.
Never rinse instruments before pre-disinfection, as this may spread microorganisms.
Insufficient or poorly performed pre-disinfection compromises the entire sterilization process:
It promotes biofilm formation, which is difficult to remove.
It increases the risk of cross-transmission of pathogens (HBV, HCV, HIV, multidrug-resistant bacteria).
It causes premature wear of instruments, reducing their effectiveness and longevity.

 The Steps of a Sterilization Cycle: Protocol and Best Practices
The Steps of a Sterilization Cycle: Protocol and Best Practices